Marker Name: Homocysteine
REFERENCE RANGES FOR HOMOCYSTEINE:
Laboratory reference range: 0–15 µmol/L
Functional reference range: < 7 µmol/L
DESCRIPTION:
Homocysteine does not appear to play any positive biological role other than as an amino acid intermediate in the methionine and folate cycles.1 However, elevated levels of homocysteine are associated with several disease states, including vascular diseases and cognitive disorders.2 Homocysteine auto-oxidizes in plasma to form biologically reactive products, namely homocysteine, homocysteine-mixed disulfides, and homocysteine thiolactone.3 Homocysteine and these related molecules may injure the vascular endothelium directly or by first interacting with low-density lipoproteins (LDL).4 Homocysteine may also be prothrombotic, especially in the context of acute coronary syndromes, increasing platelet accumulation and aggregation.5,6
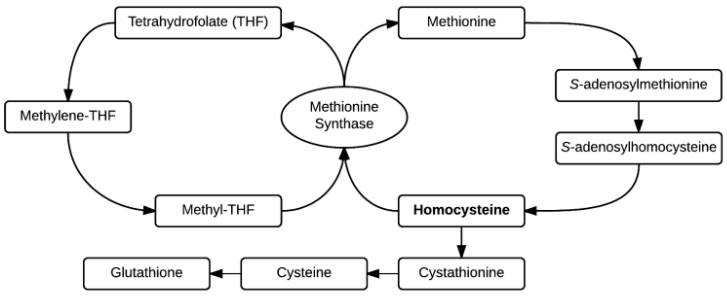
Homocysteine and methyltetrahydrofolate (methyl-THF) are substrates for methionine synthase, a vitamin B12-dependent enzyme that forms tetrahydrofolate (THF) and methionine.2 Homocysteine can also enter the transsulfuration pathway, where it is converted to cystathionine and then cysteine and glutathione through vitamin B6-dependent enzymes.7 Thus, a deficiency in folate (a precursor of methyl-THF) and/or vitamin B12 (a cofactor for methionine synthase) can interfere with methionine synthase activity, resulting in increased homocysteine, decreased methionine, and increased metabolism through the transsulfuration pathway.8
Hyperhomocysteinemia is an abnormally high level of homocysteine in the blood, as measured by plasma homocysteine. For reasons described above, the level of circulating homocysteine is inversely correlated with levels of folate, vitamin B12, and vitamin B6.9 Therefore, deficiencies in these vitamins, especially folate, may cause plasma levels of homocysteine to rise. Homocysteine levels also rise in response to diminished hormone levels, namely thyroid hormone and estrogen. Consequently, hyperhomocysteinemia has been noted in hypothyroidism and menopause.2 Plasma homocysteine levels tend to rise in patients with end-stage renal disease. Genetic diseases of impaired homocysteine metabolism, such as thermolabile methylenetetrahydrofolate reductase (MTHFR) deficiency, may raise plasma homocysteine levels.10
Plasma homocysteine may be measured with assays of serum vitamin B12, folate, and vitamin B6. A methylmalonic acid test may help distinguish between vitamin B12 or folate deficiencies.12 In folate deficiency, homocysteine levels in the serum will be abnormally high but methylmalonic acid levels will be normal. In vitamin B12 deficiency, both serum homocysteine and methylmalonic acid levels will be elevated.12
PATHOLOGICAL/CONVENTIONAL RANGE INDICATIONS:
High in:1,2,10,13,14
- Nutrient imbalances
- Vitamin B12 deficiency
- Vitamin B6 deficiency
- Folate deficiency
- Hypothyroidism
- Menopause
- Impaired homocysteine metabolism (e.g., methylenetetrahydrofolate reductase (MTHFR) mutation, cystathionine-beta-synthase deficiency)
- End-stage renal disease
Low in:
- Not applicable
FUNCTIONAL RANGE INDICATIONS:
High in:
- Same as conventional indications
Low in:
- Same as conventional indications
References:
- http://www.uptodate.com/contents/overview-of-homocysteine
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716415/
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC507392/
- http://www.ncbi.nlm.nih.gov/pubmed?term=8597939
- http://circ.ahajournals.org/content/101/4/372.abstract
- http://www.ncbi.nlm.nih.gov/pubmed?term=3628965
- http://circ.ahajournals.org/content/94/9/2154.abstract
- https://labtestsonline.org/understanding/analytes/homocysteine/tab/test/
- http://www.ncbi.nlm.nih.gov/pubmed?term=8133587
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1682970/
- http://jn.nutrition.org/content/137/2/311.abstract
- http://www.uptodate.com/contents/diagnosis-and-treatment-of-vitamin-b12-and-folate-deficiency
- http://www.ncbi.nlm.nih.gov/books/NBK114302/
- http://ajcn.nutrition.org/content/86/5/1563S.abstract