Marker Name: Iron Saturation
REFERENCE RANGES FOR IRON SATURATION:
Laboratory reference range: 15–55%
Functional reference range: 17–45%
DESCRIPTION:
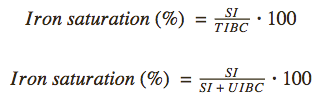
Iron saturation, also referred to as transferrin saturation (TSAT), is the percent of iron-binding sites on plasma proteins occupied by iron. Since transferrin carries the majority of plasma iron, iron saturation approximates the percent of transferrin bound by iron. To know the exact transferrin-specific saturation, direct measurement of transferrin would be required. Iron saturation is typically calculated from serum iron (SI) and total iron-binding capacity (TIBC) or unsaturated iron-binding capacity (UIBC) using one of the equations below.1
Iron saturation depends on serum iron and transferrin concentration and is therefore affected by the same variables: iron homeostasis, nutritional status, inflammation, liver function, pregnancy, certain genetic conditions, and certain drugs. For information on how these factors alter plasma transferrin and iron content, see TIBC and iron reference sheets. Note that when more than one of these health variables is simultaneously abnormal, iron saturation can be unpredictable.2 For example, a patient with concomitant protein and iron deficiency may present with normal, low, or high iron saturation.3
Iron saturation follows a diurnal rhythm, with higher values in the morning and lower values at night; however, these variations are not typically large enough to change diagnosis outcome.4,5 When iron saturation exceeds 80 percent, non-transferrin bound iron (NTBI) is found in plasma, which produces reactive oxygen species (ROS) and causes cellular damage.6,7
High iron saturation can be caused by hereditary hemochromatosis, multiple infusions of iron-containing agents, massive increase in oral iron intake, hypotransferrinemia, pernicious anemia, ineffective erythropoiesis, and some cases of hemolytic anemia, hemosiderosis, and chronic liver disease.8-21 A list of specific conditions that can cause high iron saturation is provided below.
Low iron saturation can be caused by iron deficiency, pregnancy, states of increased erythropoiesis, certain drugs, states of acute inflammation, and some cases of chronic inflammation.8-11,22-30 A full list of conditions and drugs that can cause low iron saturation is found below.
To determine the etiology of abnormal iron saturation, related iron markers should be considered, including a complete blood count (CBC), serum iron, ferritin, TIBC, and UIBC.8
PATHOLOGICAL/CONVENTIONAL RANGE INDICATIONS:
High in:8-11
- Hereditary hemochromatosis (HH)12,13
- Human hemochromatosis protein (HFE)-related
- C282Y homozygosity
- C282Y/H63D compound heterozygosity
- Other mutations of HFE
- Other genetic mutation
- Juvenile hemochromatosis (mutations in hemojuvelin or hepcidin)
- Transferrin receptor 2 mutation (rare)
- Multiple infusions of iron-containing agents
- Red cell transfusion
- Multiple infusions of intravenous iron
- Intravenous hemin/hematin
- Massive increase in oral iron intake
- High-dose iron supplementation
- Medications containing iron
- Diet
- Hypotransferrinemia
- Hereditary atransferrinemia
- Nephrotic syndrome
- Pernicious anemia14
- Ineffective erythropoiesis
- Hereditary sideroblastic anemias15
- Severe alpha and beta thalassemia16,17
- Myelodysplastic syndrome (MDS) variants, such as refractory anemia with ringed sideroblasts (RARS)18
- Hemolytic anemia (can be high, but sometimes normal)
- Autoimmune hemolytic anemia
- Sickle cell anemia
- Hemosiderosis (can be high, but sometimes normal)
- Pulmonary hemosiderosis (as seen in anti-glomerular basement membrane antibody disease)
- Chronic hemolysis
- Chronic liver disease (can be high, but sometimes normal)
- Hepatitis B or C
- Alcohol-induced liver disease19
- Porphyria cutanea tarda20
- Steatohepatitis (fatty liver disease)21
- Human hemochromatosis protein (HFE)-related
Low in:8-11,22,23
- Normal pregnancy (in the absence of iron deficiency)
- Iron deficiency
- Inadequate dietary intake (e.g., diet low in meat)
- Gastrointestinal malabsorption
- Hypochlorhydria
- Gastritis (e.g., atrophic gastritis, autoimmune metaplastic atrophic gastritis, Helicobacter pylori gastritis)
- Celiac disease
- Post-gastric bypass surgery24
- Blood loss25
- Obvious bleeding (e.g., external wound, melena, hematemesis, hemoptysis, gross hematuria)
- Heavy menstrual bleeding
- Gastrointestinal bleeding (e.g., hemorrhoids, fissures)
- Repeated blood donations
- Intraluminal neoplasms (e.g., malignancies of the gastrointestinal tract)26
- Lasthénie de Ferjol syndrome
- States of increased red blood cell production
- Treatment with erythropoietin (EPO)27
- Polycythemia vera28
- States of acute inflammation, as seen in:
- Myocardial infarction
- Sepsis
- Chronic inflammation (can be low, but often normal)29
- Multiple causes (e.g., chronic infection, malignancy, rheumatologic disorders, inflammatory bowel disease, acute and chronic immune activation, etc.)
- Drugs30
- Oral contraceptives
- Proton pump inhibitors
- H2 receptor blockers
- Certain antibiotics (e.g., quinolones, tetracycline)
- Excessive calcium supplementation
FUNCTIONAL RANGE INDICATIONS:
High in:
- Functional iron overload
- Functional liver problems
Low in:
- Functional iron deficiency
- Chronic inflammation
References:
- https://labtestsonline.org/understanding/analytes/tibc/tab/sample/
- https://books.google.com/books?id=CpXVAwgOv7sC&pg=PT103&lpg=PT103&dq=malnutrition+transferrin+saturation&source=bl&ots=rYWDIGyhZl&sig=ad5yHlTS7cN4bS8l_7C8uPdh9Es&hl=en&sa=X&ved=0CFgQ6AEwCWoVChMI0uvypfn_yAIVyFYeCh0CoQVf#v=onepage&q=malnutrition%20transferrin%20saturation&f=false
- http://www.jpgmonline.com/article.asp?issn=0022-3859;year=1981;volume=27;issue=1;spage=12;epage=5;aulast=Agarwal
- http://www.ncbi.nlm.nih.gov/pubmed/12542499
- http://www.ncbi.nlm.nih.gov/pubmed/12090432
- http://www.clinchem.org/content/48/2/307?ijkey=ec909eb75ebb57b30c63c89a5dc601c9d517b4ad&keytype2=tf_ipsecsha
- http://www.ncbi.nlm.nih.gov/pubmed/19006228?access_num=19006228&link_type=MED&dopt=Abstract
- http://unitedlabservice.com/comprehensive-lab-tests/iron-and-total-iron-binding-capacity-tibc/
- http://www.irondisorders.org/Websites/idi/files/Content/854256/HowdoIknow_Anemia__Converted_.pdf
- http://ucsdlabmed.wikidot.com/chapter-15#toc10
- http://www.aafp.org/afp/2010/1101/p1117.html
- http://www.uptodate.com/contents/genetics-of-hereditary-hemochromatosis
- http://www.uptodate.com/contents/iron-overload-syndromes-other-than-hereditary-hemochromatosis
- http://sickle.bwh.harvard.edu/fe-def.html http://www.irondisorders.org/Websites/idi/files/Content/854256/HowdoIknow_Anemia__Converted_.pdf
- http://www.uptodate.com/contents/pathophysiology-of-the-sideroblastic-anemias
- http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-the-thalassemias
- http://www.ncbi.nlm.nih.gov/pubmed/19006228?access_num=19006228&link_type=MED&dopt=Abstract
- http://www.bloodjournal.org/content/124/6/873?sso-checked=true
- http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-alcoholic-fatty-liver-disease-and-alcoholic-cirrhosis
- http://www.irondisorders.org/Websites/idi/files/Content/854256/HowdoIknow_Anemia__Converted_.pdf
- http://www.uptodate.com/contents/epidemiology-clinical-features-and-diagnosis-of-nonalcoholic-fatty-liver-disease-in-adults
- http://www.uptodate.com/contents/causes-and-diagnosis-of-iron-deficiency-anemia-in-the-adult
- http://www.uptodate.com/contents/approach-to-the-adult-patient-with-anemia
- https://www.nlm.nih.gov/medlineplus/ency/article/000584.htm
- http://www.uptodate.com/contents/anemia-caused-by-low-iron-beyond-the-basics
- http://www.uptodate.com/contents/hematologic-complications-of-malignancy-anemia-and-bleeding
- http://www.bloodjournal.org/content/96/3/823?sso-checked=true
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2772882/
- http://www.uptodate.com/contents/anemia-of-chronic-disease-inflammation
- http://www.uptodate.com/contents/treatment-of-the-adult-with-iron-deficiency-anemia