Marker Name: LDL
REFERENCE RANGES FOR LDL:
Laboratory reference range: 0–99 mg/dL
Functional reference range: 50–140 mg/dL
DESCRIPTION:
Low-density lipoprotein (LDL) is one of the five major lipoproteins; it is the major carrier of cholesterol (as cholesterol esters), and it may also carry triglycerides and phospholipids.1,2 LDL provides cholesterol to the liver for the creation of bile acids and to non-liver tissue for the synthesis of hormones, incorporation into cell membranes, and storage.3,4 Delivery of cholesterol esters in liver and non-liver tissues takes place through receptor-mediated endocytosis.5 Strictly speaking, LDL refers to the lipoprotein rather than the cholesterol. The cholesterol particle is LDL cholesterol (LDL-C). In clinical settings, LDL and LDL-C are used interchangeably, however, and both refer to LDL cholesterol.
LDL may enter the bloodstream through dietary intake or de novo synthesis in the liver. Ingested lipids are initially incorporated into chylomicrons, which deliver triglycerides to tissues.1 Chylomicrons that have been depleted of their triglycerides become chylomicron remnants and are taken up by the liver. The liver then uses these remnants to form very-low-density lipoproteins (VLDLs), which become intermediate-density lipoproteins (IDLs) in the bloodstream. A portion of VLDLs and IDLs are then converted into LDL particles.1,3 The majority of cholesterol is synthesized by the body, mostly in liver and, to a lesser degree, in the intestines.5 LDL contains apolipoprotein B-100 (Apo B-100) and apolipoprotein C-III (Apo C-III).1,2 Apo B-100 is a ligand for the LDL receptor in the liver, and Apo C-III inhibits triglyceride hydrolysis by lipoprotein lipase and hepatic lipase.1,6,7
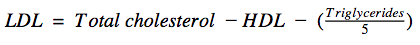
Total cholesterol, HDL cholesterol, and triglycerides are measured directly from serum or plasma samples, while LDL cholesterol is determined by mathematical calculation using measured values.2,8 The Friedewald formula is used to calculate the LDL level in blood:9
Direct measurement of LDL is more accurate than using the Friedewald formula, but considerably more expensive.8,10 In most clinical situations, a mathematical estimate is sufficient. In some patients, however, such as people with very high triglyceride levels (>400 mg/dL or >4.516 mmol/L), estimation is far too inaccurate, which usually necessitates direct measurement of LDL. Fortunately, a new calculation method that scales measurements based on the triglyceride-to-VLDL ratio may permit accurate LDL estimation in all patients without the increased expense of direct LDL measurements.11
When LDL cholesterol is elevated due to a primary genetic disorder, it may be referred to as hyperbetalipoproteinemia.12 Non-familial causes of elevated LDL cholesterol do not typically share this moniker. Causes of high LDL cholesterol that are potentially modifiable through behavioral change include sedentary lifestyle, obesity, and excessive alcohol use. LDL cholesterol levels, as well as all other lipid levels, can be expected to increase in later stages of normal pregnancy to meet increased energy demands of the mother and the fetus.13 Certain diseases of the kidney and liver can elevate LDL cholesterol levels. Endocrine diseases such as hypothyroidism and diabetes mellitus, especially type 2 diabetes, may raise LDL cholesterol levels. Various prescription and nonprescription drugs have been shown to cause elevated LDL cholesterol in some individuals.
A low LDL cholesterol level in the blood is sometimes referred to as hypobetalipoproteinemia; however, this term is usually reserved for primary causes of low LDL cholesterol, such as abetalipoproteinemia and familial hypobetalipoproteinemia. Secondary causes of low LDL cholesterol are far more common than primary causes.14 Acute and chronic infections as well as chronic inflammatory states can lower levels of circulating LDL. Severe nutritional deficits, anemia, and neutropenia may also lower LDL cholesterol. Iatrogenic causes of low LDL cholesterol include supratherapeutic doses of statins, bile acid sequestrants, or ezetimibe.
LDL cholesterol is measured as part of the standard serum lipid profile. The serum lipid profile includes total cholesterol, HDL cholesterol, and triglycerides. This report may also provide calculated estimates of VLDL cholesterol, non-HDL cholesterol, and the cholesterol/HDL ratio.15
PATHOLOGICAL/CONVENTIONAL RANGE INDICATIONS: High in:13,16
- Primary causes
- Heterozygous familial hypercholesterolemia
- Homozygous familial hypercholesterolemia
- Polygenic hypercholesterolemia
- Primary hyperlipoproteinemia type 1
- Normal pregnancy (third trimester)
- Obesity
- Sedentary lifestyle
- Alcohol abuse
- Diabetes mellitus
- Hypothyroidism
- Chronic kidney disease
- Nephrotic syndrome
- Cholestatic liver diseases
- Drugs
- Anabolic steroids
- Thiazides
- Beta-blockers
- Retinoids
- Glucocorticoids
- Highly active antiretroviral agents
- Oral estrogens
- Anti-rejection drugs
Low in:14
- Primary causes
- Abetalipoproteinemia
- Hypobetalipoproteinemia
- Chylomicron retention disease
- Infection
- Chronic (e.g., hepatitis C)
- Acute
- Hyperthyroidism
- Anemia
- Malnourishment
- Anorexia
- Malabsorption
- Poor diet
- Neutropenia
- Advanced, non-cholestatic liver disease
- Malignancy
- Drugs
- Statins
- Bile acid sequestrants
- Ezetimibe
FUNCTIONAL RANGE INDICATIONS:
High in:
- Same as conventional indications
- Poor thyroid function
- Intestinal permeability
- Chronic infections
- Heavy metal toxicity (and possibly presence of other toxins such as mold)
Low in:
- Same as conventional indications
References:
- http://www.uptodate.com/contents/lipoprotein-classification-metabolism-and-role-in-atherosclerosis
- http://www.uptodate.com/contents/measurement-of-blood-lipids-and-lipoproteins
- http://www.utmb.edu/pedi_ed/Obesity/page_19.htm
- http://circ.ahajournals.org/content/108/22/2751.abstract
- http://www.ncbi.nlm.nih.gov/books/NBK22336/
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3244212/
- http://www.ncbi.nlm.nih.gov/pubmed/?term=3621516
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4687457/
- http://www.clinchem.org/content/18/6/499.abstract
- http://www.ncbi.nlm.nih.gov/pubmed?term=23524048
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4226221/
- http://www.ncbi.nlm.nih.gov/pubmed/21712784
- http://press.endocrine.org/doi/abs/10.1210/jcem.85.12.7027
- http://merckmanuals.com/professional/endocrine-and-metabolic-disorders/lipid-disorders/hypolipidemia
- https://labtestsonline.org/understanding/analytes/lipid/tab/test/
- http://merckmanuals.com/professional/endocrine-and-metabolic-disorders/lipid-disorders/dyslipidemia