Marker Name: Reverse T3
REFERENCE RANGE FOR REVERSE T3 (TRIIODOTHYRONINE):
Laboratory reference range: 9.2–24.1 ng/dL
DESCRIPTION:
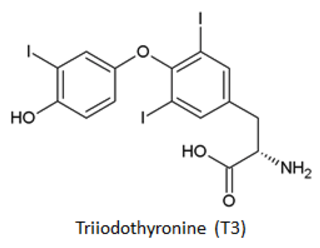
Reverse triiodothyronine (reverse T3; rT3) does not stimulate nuclear thyroid hormone receptors and, as such, is considered an inactive thyroid hormone. While rT3 possesses no direct thyroid hormone effect, the molecule is a competitive inhibitor of enzymatic conversion of T4 to T3.1
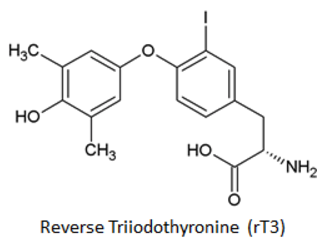
Reverse T3 may also play several minor biological roles.2 For example, rT3 potently initiates actin polymerization in astrocytes, which means it plays a potentially critical role in brain development.3 Reverse T3 also inhibits the release of free fatty acids normally stimulated by dexamethasone or adrenaline.4
Serum rT3 levels do not increase in response to TSH, as T3 and T4 levels do, suggesting that thyroid secretion of rT3 is negligible. Conversion of T4 to rT3 in peripheral tissues is the main way rT3 is synthesized.5 Two major forms of thyroxine-5′-deiodinases (type I and type II) are responsible for converting free T4 into the more active thyroid hormone, T3.6 While type I can also convert T4 into rT3, a third thyroxine-5′-deiodinase (type III) is primarily responsible for this enzymatic conversion.6-8 Type III thyroxine-5′-deiodinase is found in virtually every peripheral tissue except the pituitary gland. The enzyme is particularly important during fetal development, but it is normally undetectable in adult tissues.9 However, recent work with sensitive assays shows that type III is also present in adult tissues, especially neurons, and increases dramatically after tissue injury or during severe illness.7,9
Type III thyroxine-5′-deiodinase activity is increased during hyperthyroidism and decreased during hypothyroidism, leading to relative increases and decreases in rT3 levels, respectively. This deiodinase is induced in tissues that have been injured or are suffering from hypoxia.9 Conversely, growth hormone and glucocorticoids reduce the activity of this enzyme. In addition to converting T4 into rT3, type III thyroxine-5′-deiodinase also inactivates T3, converting it into 3,3′-diiodothyronine (T2).7 Both type I and type II thyroxine-5′-deiodinases convert rT3 into T2.10
Most causes of elevated rT3 are due to changes in the activity of type III thyroxine-5′-deiodinase.11,12 Any serious illness can induce the activity of this enzyme, but hypoxia and ischemia appear to be particularly potent.13 Type III thyroxine-5′-deiodinase activity increases as does the level of serum rT3 in protein calorie malnutrition, carbohydrate deprivation, chronic renal failure, cirrhosis, and uncontrolled diabetes. Non-thyroidal illness syndrome (i.e., euthyroid sick syndrome) is recognized by low T3 and T4 concentrations with elevated rT3 levels in the context of inappropriately low or unchanged thyroid-stimulating hormone (TSH) levels.14
Any state that suppresses the action of type III thyroxine-5′-deiodinase would, in turn, decrease serum rT3 levels. In practical terms, this only occurs in patients with hypothyroidism or those being treated with growth hormones or glucocorticoids.7 Individuals with a rare genetic defect called X-linked monocarboxylate transporter 8 deficiency effectively have reduced type III thyroxine-5′-deiodinase activity and low rT3 levels.11,15
Serum rT3 levels are most useful in a clinical setting as a means of distinguishing between nonthyroidal illness and a primary thyroid disease.12 In patients with central hypothyroidism, rT3 levels are low because of reduced amounts of substrate, namely T4. On the other hand, Type III thyroxine-5′-deiodinase activity is induced by severe illness, especially hypoxia or ischemia, which will increase serum rT3 levels.
Thyroxine sulfate levels may also be measured with rT3; thyroxine sulfate is elevated in severe nonthyroidal illness.16 Serum rT3 levels are usually only measured in the context of a thyroid function work-up including total T3, total T4, free T4, TSH, etc.12,17,18
PATHOLOGICAL/CONVENTIONAL RANGE INDICATIONS:
High in:5,11,14,19,20
- Carbohydrate deprivation
- Malnutrition
- Hyperthyroidism
- Non-thyroidal illness syndrome (i.e., euthyroid sick syndrome)
- Inflammation
- Cirrhosis
- Chronic renal failure
- Acute febrile illness
- Uncontrolled diabetes mellitus
- Drugs
- Amiodarone
Low in:12,13,15
- Central hypothyroidism
- X-linked monocarboxylate transporter 8 deficiency
- Drugs
- Growth hormone
- Glucocorticoids
FUNCTIONAL RANGE INDICATIONS:
High in:
- Same as conventional indications
Low in:
- Same as conventional indications
References:
- http://press.endocrine.org/doi/abs/10.1210/endo-101-2-453
- http://joe.endocrinology-journals.org/content/221/2/R1.abstract
- http://www.ncbi.nlm.nih.gov/pubmed/16469804
- http://www.ncbi.nlm.nih.gov/pubmed/12019951
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC333152/
- http://www.uptodate.com/contents/thyroid-hormone-synthesis-and-physiology
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3673746/
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190373/
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3133953/
- http://dx.doi.org/10.1039/C3MT00185G
- http://www.ncbi.nlm.nih.gov/pubmed/16174716
- http://www.uptodate.com/contents/thyroid-function-in-nonthyroidal-illness
- http://www.ncbi.nlm.nih.gov/pubmed?term=12843166
- http://joe.endocrinology-journals.org/content/225/3/R67.abstract
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3959653/
- http://www.ncbi.nlm.nih.gov/pubmed?term=16189257
- http://www.uptodate.com/contents/laboratory-assessment-of-thyroid-function
- http://www.uptodate.com/contents/diagnosis-of-and-screening-for-hypothyroidism-in-nonpregnant-adults
- http://www.ncbi.nlm.nih.gov/pubmed/15114257
- http://www.ncbi.nlm.nih.gov/pubmed/7148329