Marker Name: Total T3
REFERENCE RANGES FOR TOTAL T3 (TRIIODOTHYRONINE):
Laboratory reference range: 71–180 ng/dL
Functional reference range: 100–180 ng/dL
DESCRIPTION:
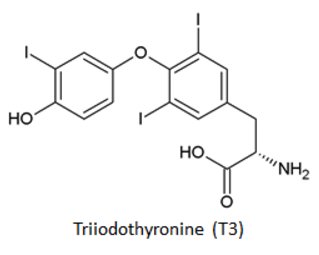
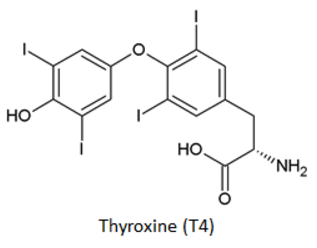
Triiodothyronine (T3) is the major biologically active thyroid hormone.1 Thyroid hormone alters the rate of protein synthesis and substrate turnover of essentially every cell in the body by directly driving gene transcription.2 Thyroid hormone is critical for early human development and cellular activity throughout life. Serious and long-term developmental delays can occur if insufficient thyroid hormone is available to a developing fetus, neonate, or child. Likewise, too much or too little circulating thyroid hormone causes various health issues in adults.3,4 Therefore, several physiological mechanisms exist to tightly control the synthesis and secretion of thyroid hormone.5
Approximately 20 percent of T3 is synthesized and secreted by the thyroid gland, while the remaining 80 percent comes from the enzymatic conversion of T4 (thyroxine) to T3 in peripheral tissues.5 Thyroid-stimulating hormone (TSH, also called thyrotropin) controls virtually every step of thyroid hormone synthesis and secretion in the thyroid gland and drives peripheral conversion of T4 to T3. T4 is converted to T3 by several thyroxine-5′-deiodinase enzymes.5 Factors that influence thyroxine-5′-deiodinase activity include the presence of thyroid hormone, nutritional status, and acute illness.
T3 acts at nuclear receptors to alter gene transcription. It is thought that only free T3 (i.e., T3 that is not bound to serum proteins) can be taken up by cells and affect nuclear thyroid hormone receptors. Therefore, only free T3 is considered biologically active at any moment. A mere 0.5 percent of T3 in the serum is in this active state. The remaining 99.5 percent of T3 in the serum is bound to serum proteins; 80 percent is bound to thyroxine-binding globulin (TBG), 5 percent is bound to transthyretin (TTR), and 15 percent is bound to albumin and lipoprotein.5
Changes in the concentration of serum-binding proteins can have a substantial effect on total T3 concentrations in the blood.5 Increased TBG concentrations (e.g., from estrogens, hepatitis, etc.) will increase total T3, while abnormally low levels of TBG (e.g., from anabolic steroids, nephrotic syndrome, etc.) will lower total T3.6 Under most circumstances, serum-binding protein levels do not alter free T3 hormone concentrations or the absolute rate of T3 metabolism.5,6 Consequently, serum total T3 concentrations may vary substantially based on serum protein concentrations but do not necessarily change free T3 concentrations in the blood.6
Elevated total T3 levels usually indicate hyperthyroidism or a euthyroid state in which serum protein levels are increased.4,6,7 Drugs that increase TBG levels will increase total T3 levels.6 Thyroid physiology changes during the course of normal pregnancy to meet the needs of the mother and the fetus. Consequently, total T3 concentrations rise during the first 20 weeks of gestation, reaching a new plateau level for the remainder of the pregnancy.8
Decreased total T3 levels in the serum may be present in individuals with hypothyroidism or chronic thyroiditis. Deficiency in serum-binding proteins will also result in decreased total T3 levels. This may occur in patients with nephrotic syndrome, who may pass substantial amounts of serum proteins in the urine, consequently lowering TBG and total T3 levels.9 High levels of circulating androgens, glucocorticoids, cortisol, or growth hormone can also lower TBG levels, and therefore total T3 levels.6,10
Total T3 is often ordered with other thyroid markers, including TSH, total T4, free T3, and free T4.11-13
PATHOLOGICAL/CONVENTIONAL RANGE INDICATIONS:
High in:6,8,14-16
- Normal pregnancy
- Hyperthyroidism
- Euthyroid hyperthyroxinemia
- T3 toxicosis
- Acute thyroiditis
- Familial dysalbuminemic hyperthyroxinemia
- Drugs that increase TBG (e.g., estrogens, tamoxifen, opioids)
- Synthetic triiodothyronine treatment
Low in:6,14,15
- Hypothyroidism
- Chronic thyroiditis
- Subacute thyroiditis
- Nephrotic syndrome
- Endocrine disorders that decrease TBG
- Cushing syndrome
- Acromegaly
- Uncontrolled diabetes mellitus
- Drugs that decrease TBG (e.g., anabolic steroids, glucocorticoids)
FUNCTIONAL RANGE INDICATIONS:
High in:
- Hyperthyroidism
- Facetious hyperthyroidism (excess thyroid hormone replacement)
Low in:
- Hypothyroidism
- Inflammation
References:
- http://www.ncbi.nlm.nih.gov/books/NBK285568/
- http://www.uptodate.com/contents/thyroid-hormone-action
- http://www.uptodate.com/contents/diagnosis-of-and-screening-for-hypothyroidism-in-nonpregnant-adults
- http://www.uptodate.com/contents/diagnosis-of-hyperthyroidism
- http://www.uptodate.com/contents/thyroid-hormone-synthesis-and-physiology
- http://www.uptodate.com/contents/euthyroid-hyperthyroxinemia-and-hypothyroxinemia
- http://emedicine.medscape.com/article/118562-overview
- http://www.uptodate.com/contents/overview-of-thyroid-disease-in-pregnancy
- http://dx.doi.org/10.7326/0003-4819-90-3-335
- http://www.ncbi.nlm.nih.gov/pubmed?term=3903380
- http://www.mayomedicallaboratories.com/test-catalog/Overview/8613
- http://www.mayomedicallaboratories.com/test-catalog/Overview/9404
- http://www.uptodate.com/contents/disorders-that-cause-hyperthyroidism
- http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/8724
- http://www.uptodate.com/contents/laboratory-assessment-of-thyroid-function
- http://www.amjmed.com/article/S0002-9343%2805%2900219-6/abstract